This generation is characterized by its extremely active lifestyle and breakneck pace. The forerunners in this race are teenagers. Armed with their gargantuan passion, zeal, and motivation, teenagers don’t want to stop at all. They want it all, and they want it fast. This leads to adopting an unhealthy lifestyle. One that boosts productivity but takes a toll on the body and its well-being. People between the ages group of 18-25 are most susceptible to this. Their extremely busy schedule leaves them with almost no time to rest. Their machine-like functioning body thus starts giving signals that it needs oiling and maintenance. These signals are in the form of various physical ailments. The most common grievance being back pain.

Teenagers and young adults are often found complaining about having the back of a 90-year old. They believe it is just them, but research shows otherwise. The chances of experiencing LBP (low back pain) are almost as high as 80% by the time one gets to the age of 20.
Causes of Back Pain in Teenagers: –
Back pain in teenagers can be of different types and have different sources of origin. The nature of back pain depends on the lifestyle and also sometimes on genetics. Here are some of the major causes and forms of back pain.
- Muscle-Related Pain
This an external affliction of the muscles surrounding the spinal cord region. It does not involve the spinal cord itself. It is primarily focused near the thoracic and lumbar regions. This pain is characterized by continuous resonating pain. It usually disappears after proper resting and when the strained muscles are relaxed. Improper posture, carrying a heavy load, faulty sports equipment, psychosocial distress, anxiety and in some cases, even a past injury can cause such pain.
- Spondylolysis
Spondylolysis is caused when a gap formation or separation takes place between vertebral bones. It is a common occurrence in young athletes and teenagers who tend to hyperextend their backs.
- Spondylolisthesis
This is an acute condition in which one vertebra slips on top of the other. It can lead to chronic pain, and if not treated, immediately made lead to permanent deformity. It might need spinal infusion and surgery at a later point.
- Disc Injuries and vertebral fractures
A fracture in the vertebra can be a result of some sudden shock or impact. This could occur while engaging in some extreme sports, gymnastics, or being involved in an accident. Damage to the vertebra or the intervertebral discs needs to attended immediately. Surgical procedures to prevent further damage to the area of fracture becomes a necessity.
- Other Causes
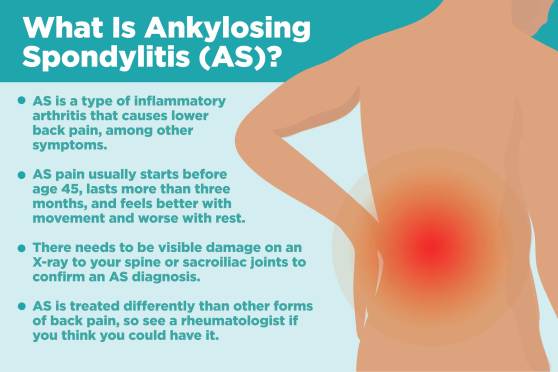
Some other causes of chronic back pain could the presence of a spinal tumor, an infection, or inflammatory arthritis.
Spinal Fractures

In this article, we shall take a closer look at the bone-related injuries in the spinal cord. To be more specific fractures, cracks, and deformities in the spine. The spine is one of the most essential parts of our body. It protects the spinal cord, which relays the information from the brain to the different parts of our body. Damage to the spine can even lead to partial and complete paralysis. Thus, it is imperative to ensure that the spine stays protected from serious injuries. Immediate medical attention must be provided to prevent grievous harm to our bodies.
Symptoms
A fracture in the spine is detected using an X-ray. However, certain early signs and symptoms can help identify a fracture. These symptoms include back pain, muscle cramps, severe neck pain, weakness, partial or complete paralysis.
Causes
A fracture in the spine most commonly occurs when the person is involved in some accident. In fact, car accidents make up 45% of spinal cord related injuries. Extreme sports, falling, and improper posture are some other causes of a spinal fracture.
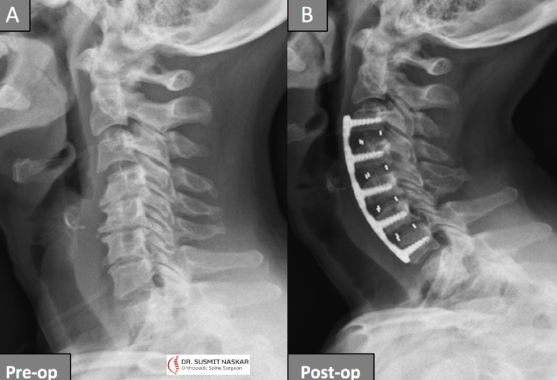
Diagnosis
Once the symptoms are experienced, the patient needs to visit a hospital or a nursing home. There the spinal fracture can be detected with the help of an X-ray, CT scan, or MRI scan. These are medical imaging techniques that help the doctors to take a look at the bone structure.
Types of Spinal Fracture
- Compression Fracture – This kind of fracture is prevalent among people suffering from osteoporosis. Owing to weak bone structure, a sudden shock or impact results in a fracture in the vertebra. A special case in which the front part bends under pressure is called wedge fracture, due to the wedge-shaped deformity.
- Burst Fracture – Burst fracture is a result of a severe accident like a car crash. The spine gets completely crushed, and a lot of vertebrae are fractured. The bone breaks into pieces in several regions. These fragments pose a threat of causing damage to the spinal cord.
- Fracture Dislocation – A fracture in the spine can lead to certain vertebrae from getting dislocated. When the body is involved in an accident, the vertebra can shift from its original position and lead to a fracture-dislocation.
Treatments Available
Treatments can be broadly categorized into surgical and non-surgical procedures.
Surgical Procedures
- ANTERIOR CERVICAL DISCECTOMY AND FUSION (ACDF)
This form of treatment is offered to the patients suffering from a cervical slip disc. The procedure requires an incision to reach the affected area and remove the disk to decompress the spine and relief the tension from the nerves. An artificial replacement is provided in place of the removed cervical disc to offer stability to the structure of the spine.
- CERVICAL LAMINOPLASTY
This procedure is an ideal treatment for those who suffer from myelopathy or compression of the spinal cord. The spinal cord of the patient undergoes an ‘extension’ or ‘stretch’ from one side of the spine to another, as well as from top to bottom, to release the pressure from the spinal cord. It also gradually reduces strain from the nerves and prevents any complication.
- CERVICAL POSTERIOR FORAMINOTOMY
When your back suffers through pain for a prolonged period, especially after a pinched nerve, Cervical Posterior Foraminotomy is applicable. Usually, the reason is due to the compression of nerves, or a herniated disk. Hence, it becomes important to perform incision and make space for the nerves to move freely and release the tension. Thus, relieving the pain.
- LAMINECTOMY
Sometimes the spinal cord builds intense pressure. The pressure can result in intense pain, and there are several reasons for it; a herniated disk is usually the common culprit. However, the surgical procedure receives its name as it is a process of removal of lamia from the spinal canal. It releases pressure and offers relief.
- CORPECTOMY
This method is only employed when all others fail. It is performed when a person suffers through a spinal fracture, infection, or other medical condition. When all else fails, this method will remove the damaged parts like disk or vertebra, from the spine to offer relief and prevent nerves from getting compressed.
- LUMBAR DISC MICROSURGERY
The main purpose of this procedure is to relieve the patient off the excruciating leg pain, also known as Sciatica. It is a minimalistic surgical procedure in which the ‘herniated’ disk gets removed, and nerves under pressure are released.
- VERTEBROPLASTY
It is a process in which medical experts take non-surgical measures and offer opportunities to strengthen the vertebra of the spine.
- SCOLIOSIS CORRECTION SURGERY
Scoliosis is the bending of the spine to the sideways, almost like a curve, a physical deformity. To fix the issue, the surgeon utilizes tools like screws in the defective bones and uses rods to assist in correcting the posture over time.
- KYPHOSIS CORRECTION SURGERY
Kyphosis is similar to Scoliosis. However, it is the forward bending of the spine instead of the sideways. It requires similar treatment measurements for proper recovery.
- MIS SPINAL FUSION
It is a new medical surgery where specialists use microscopic equipment to carry out the procedure. The method is least painful of all, as there are minute incisions and cuts, barely felt, after the surgery. It is a perfect option for patients that are obese or overweight in general.
Non-Surgical Procedures
- FACET JOINT INJECTIONS
It delivers small amounts of anesthetic and steroid medication to relieve pain in the neck and back. It also helps in diagnosing and locating the source of pain to provide immediate relief.
- LUMBAR EPIDURAL STEROID INJECTION
It is a pain management procedures prevalent in the spinal surgeries and medical conditions. From severe leg pain due to spine compression and herniated disk to other deformity-based pain, it is a very efficient method. A pain management specialist will introduce anti-inflammatory and anesthetic agents to the root of the cause and offer relief.
- LUMBAR TRANSFORAMINAL EPIDURAL STEROID INJECTION
This is a pain-monitoring treatment, or known as ‘pain-treatment.’ It is usually employed when a patient is suffering through excruciating pain due to some form of spinal injury. Usually, it is due to the lumbar spine problems and requires attention to numb the pain in the legs and possibly lower back. The doctor who is in charge of the treatment will use a combination of anti-inflammatory and anesthetic injection and insert it into the main affected region (The spine) to offer relief to the patient.